Rheumatoid Arthritis
Definition of Rheumatoid Arthritis
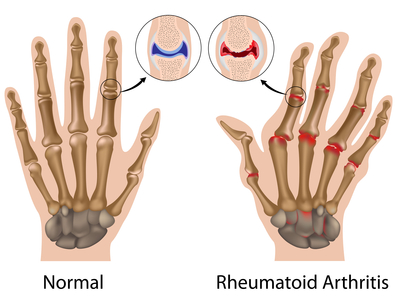
Rheumatoid arthritis (RA) is an autoimmune disease that results in a chronic, systemic inflammatory disorder that may affect many tissues and organs, but principally attacks flexible (synovial) joints. It can be a disabling and painful condition, which can lead to substantial loss of functioning and mobility if not adequately treated.
The process involves an inflammatory response of the capsule around the joints (synovium) secondary to swelling (turgescence) of synovial cells, excess synovial fluid, and the development of fibrous tissue (pannus) in the synovium. The pathology of the disease process often leads to the destruction of articular cartilage and ankylosis (fusion) of the joints. RA can also produce diffuse inflammation in the lungs, the membrane around the heart (pericardium), the membranes of the lung (pleura), and white of the eye (sclera), and also nodular lesions, most common in subcutaneous tissue. Although the cause of RA is unknown, autoimmunity plays a big part, and RA is a systemic autoimmune disease. It is a clinical diagnosis made on the basis of symptoms, physical exam, radiographs (X-rays) and labs.
Causes of Rheumatoid Arthritis
RA is a form of autoimmunity, the causes of which are still not completely known. It is a systemic (whole body) disorder principally affecting synovial tissues. There is no evidence that physical and emotional effects or stress could be a trigger for the disease. The many negative findings suggest that either the trigger varies, or that it might in fact be a chance event inherent with the immune response
Half of the risk for RA is believed to be genetic. It is strongly associated with the inherited tissue type major histocompatibility complex (MHC) antigen HLA-DR4 (most specifically DR0401 and 0404), and the genes PTPN22 and PADI4—hence family history is an important risk factor.
Inheriting the PTPN22 gene has been shown to double a person’s susceptibility to RA. PADI4 has been identified as a major risk factor in people of Asian descent, but not in those of European descent. First-degree relatives prevalence rate is 2–3% and disease genetic concordance in monozygotic twins is approximately 15–20%.
Smoking is the most significant non-genetic risk with RA being up to three times more common in smokers than non-smokers, particularly in men, heavy smokers, and those who are rheumatoid factor positive. Modest alcohol consumption may be protective.
Epidemiological studies have confirmed a potential association between RA and two herpesvirus infections:Epstein-Barr virus (EBV) and Human Herpes Virus 6 (HHV-6). Individuals with RA are more likely to exhibit an abnormal immune response to EBV and have high levels of anti-EBV antibodies.
Vitamin D deficiency is common in those with RA and may be causally associated. Some trials have found a decreased risk for RA with vitamin D supplementation while others have not.
Signs and Symptoms of Rheumatoid Arthritis
RA primarily affects joints, however it also affects other organs in 15–25% of individuals. It can be difficult to determine whether disease manifestations are directly caused by the rheumatoid process itself, or from side effects of the medications used to treat it – for example, lung fibrosis from methotrexate or osteoporosis from corticosteroids.
 Joints
Joints
Arthritis of joints involves inflammation of the synovial membrane. Joints become swollen, tender and warm, and stiffness limits their movement. With time, multiple joints are affected (it is a polyarthritis). Most commonly involved are the small joints of the hands, feet and cervical spine, but larger joints like the shoulder and knee can also be involved. Synovitis can lead to tethering of tissue with loss of movement and erosion of the joint surface causing deformity and loss of function.
RA typically manifests with signs of inflammation, with the affected joints being swollen, warm, painful and stiff, particularly early in the morning on waking or following prolonged inactivity. Increased stiffness early in the morning is often a prominent feature of the disease and typically lasts for more than an hour. Gentle movements may relieve symptoms in early stages of the disease. These signs help distinguish rheumatoid from non-inflammatory problems of the joints, often referred to as osteoarthritis or “wear-and-tear” arthritis. In arthritis of non-inflammatory causes, signs of inflammation and early morning stiffness are less prominent with stiffness typically less than 1 hour, and movements induce pain caused by mechanical arthritis. In RA, the joints are often affected in a fairly symmetrical fashion, although this is not specific, and the initial presentation may be asymmetrical.
As the pathology progresses the inflammatory activity leads to tendon tethering and erosion and destruction of the joint surface, which impairs range of movement and leads to deformity. The fingers may suffer from almost any deformity depending on which joints are most involved. Specific deformities, which also occur in osteoarthritis, include ulnar deviation, boutonniere deformity, swan neck deformity and “Z-thumb.” “Z-thumb” or “Z-deformity” consists of hyperextension of the interphalangeal joint, fixed flexion and subluxation of the metacarpophalangeal joint and gives a “Z” appearance to the thumb. The hammer toe deformity may be seen. In the worst case, joints are known as arthritis mutilans due to the mutilating nature of the deformities.
Skin
The rheumatoid nodule, which is sometimes cutaneous, is the feature most characteristic of RA. It is a type of inflammatory reaction known to pathologists as a “necrotizing granuloma”. The initial pathologic process in nodule formation is unknown but may be essentially the same as the synovitis, since similar structural features occur in both. The nodule has a central area of fibrinoid necrosis that may be fissured and which corresponds to the fibrin-rich necrotic material found in and around an affected synovial space. Surrounding the necrosis is a layer of palisading macrophages and fibroblasts, corresponding to the intimal layer in synovium and a cuff of connective tissue containing clusters of lymphocytes and plasma cells, corresponding to the subintimal zone in synovitis. The typical rheumatoid nodule may be a few millimetres to a few centimetres in diameter and is usually found over bony prominences, such as the olecranon, the calcaneal tuberosity, the metacarpophalangeal joint, or other areas that sustain repeated mechanical stress. Nodules are associated with a positive RF (rheumatoid factor) titer and severe erosive arthritis. Rarely, these can occur in internal organs or at diverse sites on the body.
Several forms of vasculitis occur in RA. A benign form occurs as microinfarcts around the nailfolds. More severe forms include livedo reticularis, which is a network (reticulum) of erythematous to purplish discoloration of the skin caused by the presence of an obliterative cutaneous capillaropathy.
Other, rather rare, skin associated symptoms include pyoderma gangrenosum, Sweet’s syndrome, drug reactions, erythema nodosum, lobe panniculitis, atrophy of finger skin, palmar erythema, diffuse thinning (rice paper skin), and skin fragility (often worsened by corticosteroid use).
Lungs
Fibrosis of the lungs is a recognized response to rheumatoid disease. It is also a rare but well recognized consequence of therapy (for example with methotrexate and leflunomide). Caplan’s syndrome describes lung nodules in individuals with RA and additional exposure to coal dust. Pleural effusions are also associated with RA. Another complication of RA is Rheumatoid Lung Disease. It is estimated that about one quarter of Americans with RA develop Rheumatoid Lung Disease.
Kidneys
Renal amyloidosis can occur as a consequence of chronic inflammation. RA may affect the kidney glomerulus directly through a vasculopathy or a mesangial infiltrate but this is less well documented (though this is not surprising, considering immune complex-mediated hypersensitivities are known for pathogenic deposition of immune complexes in organs where blood is filtered at high pressure to form other fluids, such as urine and synovial fluid). Treatment with Penicillamine and gold salts are recognized causes of membranous nephropathy.
Heart and blood vessels
People with RA are more prone to atherosclerosis, and risk of myocardial infarction (heart attack) and stroke is markedly increased. Other possible complications that may arise include: pericarditis, endocarditis, left ventricular failure, valvulitis and fibrosis. Many people with RA do not experience the same chest pain that others feel when they have angina or myocardial infarction. To reduce cardiovascular risk, it is crucial to maintain optimal control of the inflammation caused by RA (which may be involved in causing the cardiovascular risk), and to use exercise and medications appropriately to reduce other cardiovascular risk factors such as blood lipids and blood pressure. Doctors who treat RA patients should be sensitive to cardiovascular risk when prescribing anti-inflammatory medications, and may want to consider prescribing routine use of low doses of aspirin if the gastrointestinal effects are tolerable.
Other
Ocular
The eye is directly affected in the form of episcleritis which when severe can very rarely progress to perforating scleromalacia. Rather more common is the indirect effect of keratoconjunctivitis sicca, which is a dryness of eyes and mouth caused by lymphocyte infiltration of lacrimal and salivary glands. When severe, dryness of the cornea can lead to keratitis and loss of vision. Preventive treatment of severe dryness with measures such as nasolacrimal duct blockage is important.
Hepatic
Cytokine production in joints and/or hepatic (liver) Kupffer cells leads to increased activity of hepatocytes with increased production of acute-phase proteins, such as C-reactive protein, and increased release of enzymes such as alkaline phosphatase into the blood. In Felty’s syndrome, Kupffer cell activation is so marked that the resulting increase in hepatocyte activity is associated with nodular hyperplasia of the liver, which may be palpably enlarged. Although Kupffer cells are within the hepatic parenchyma, they are separate from hepatocytes. As a result there is little or no microscopic evidence of hepatitis (immune-mediated destruction of hepatocytes). Hepatic involvement in RA is essentially asymptomatic.
Hematological
Anemia is by far the most common abnormality of the blood cells which can be caused by a variety of mechanisms. The chronic inflammation caused by RA leads to raised hepcidin levels, leading to anemia of chronic disease where iron is poorly absorbed and also sequestered into macrophages. RA may also cause a warm autoimmune hemolytic anemia. The red cells are of normal size and colour (normocytic and normochromic). A low white blood cell count (neutropenia) usually only occurs in patients with Felty’s syndrome with an enlarged liver and spleen. The mechanism of neutropenia is complex. An increased platelet count (thrombocytosis) occurs when inflammation is uncontrolled.
Neurological
Peripheral neuropathy and mononeuritis multiplex may occur. The most common problem is carpal tunnel syndrome caused by compression of the median nerve by swelling around the wrist. Atlanto-axial subluxation can occur, owing to erosion of the odontoid process and/or transverse ligaments in the cervical spine’s connection to the skull. Such an erosion (>3mm) can give rise to vertebrae slipping over one another and compressing the spinal cord. Clumsiness is initially experienced, but without due care this can progress to quadriplegia.
Constitutional symptoms
Constitutional symptoms including fatigue, low grade fever, malaise, morning stiffness, loss of appetite and loss of weight are common systemic manifestations seen in patients with active RA.
Osteoporosis
Local osteoporosis occurs in RA around inflamed joints. It is postulated to be partially caused by inflammatory cytokines. More general osteoporosis is probably contributed to by immobility, systemic cytokine effects, local cytokine release in bone marrow and corticosteroid therapy.
Lymphoma
The incidence of lymphoma is increased in RA, although it is still uncommon.
Risk Factors for Rheumatoid Arthritis
- There are nearly three times as many women as men with the disease.
- Rheumatoid arthritis can occur at any age, but it most commonly begins between the ages of 40 and 60.
- Half of the risk for RA is believed to be genetic.
- Smoking is the most significant non-genetic risk
- Vitamin D deficiency is common in those with RA and may be causally associated
- The disease occurs in all ethnic groups and in every part of the world.
Diagnosis of Rheumatoid Arthritis
Imaging
X-rays of the hands and feet are generally performed in people with a polyarthritis. In RA, there may be no changes in the early stages of the disease, or the x-ray may demonstrate juxta-articular osteopenia, soft tissue swelling and loss of joint space. As the disease advances, there may be bony erosions and subluxation. X-rays of other joints may be taken if symptoms of pain or swelling occur in those joints.
Other medical imaging techniques such as magnetic resonance imaging (MRI) and ultrasound are also used in RA.
Blood tests
When RA is clinically suspected, immunological studies are required, such as testing for the presence of rheumatoid factor (RF, a non-specific antibody). A negative RF does not rule out RA; rather, the arthritis is called seronegative. This is the case in about 15% of patients. During the first year of illness, rheumatoid factor is more likely to be negative with some individuals converting to seropositive status over time. RF is also seen in other illnesses, for example Sjögren’s syndrome, Hepatitis C, chronic infections and in approximately 10% of the healthy population, therefore the test is not very specific.
Because of this low specificity, new serological tests have been developed, which test for the presence of the anti-citrullinated protein antibodies (ACPAs) or anti-CCP. Like RF, these tests are positive in only a proportion (67%) of all RA cases, but are rarely positive if RA is not present, giving it a specificity of around 95%. As with RF, there is evidence for ACPAs being present in many cases even before onset of clinical disease.
The most common tests for ACPAs are the anti-CCP (cyclic citrullinated peptide) test and the Anti-MCV assay (antibodies against mutated citrullinated Vimentin). Recently a serological point-of-care test (POCT) for the early detection of RA has been developed. This assay combines the detection of rheumatoid factor and anti-MCV for diagnosis of RA and shows a sensitivity of 72% and specificity of 99.7%.
Also, several other blood tests are usually done to allow for other causes of arthritis, such as lupus erythematosus. The erythrocyte sedimentation rate (ESR), C-reactive protein, full blood count, renal function, liver enzymes and other immunological tests (e.g., antinuclear antibody/ANA) are all performed at this stage. Elevated ferritin levels can reveal hemochromatosis, a mimic of RA, or be a sign of Still’s disease, a seronegative, usually juvenile, variant of rheumatoid arthritis.
Differential diagnoses
Several other medical conditions can resemble RA, and usually need to be distinguished from it at the time of diagnosis:
- Crystal induced arthritis (gout, and pseudogout) – usually involves particular joints (knee, MTP1, heels) and can be distinguished with aspiration of joint fluid if in doubt. Redness, asymmetric distribution of affected joints, pain occurs at night and the starting pain is less than an hour with gout.
- Osteoarthritis – distinguished with X-rays of the affected joints and blood tests, age (mostly older patients), starting pain less than an hour, a-symmetric distribution of affected joints and pain worsens when using joint for longer periods.
- Systemic lupus erythematosus (SLE) – distinguished by specific clinical symptoms and blood tests (antibodies against double-stranded DNA)
- One of the several types of psoriatic arthritis resembles RA – nail changes and skin symptoms distinguish between them
- Lyme disease causes erosive arthritis and may closely resemble RA – it may be distinguished by blood test in endemic areas
- Reactive arthritis (previously Reiter’s disease) – asymmetrically involves heel, sacroiliac joints, and large joints of the leg. It is usually associated with urethritis, conjunctivitis, iritis, painless buccal ulcers, and keratoderma blennorrhagica.
- Ankylosing spondylitis – this involves the spine, although a RA-like symmetrical small-joint polyarthritis may occur in the context of this condition.
- Hepatitis C – RA-like symmetrical small-joint polyarthritis may occur in the context of this condition. Hepatitis C may also induce Rheumatoid Factor auto-antibodies
Rarer causes that usually behave differently but may cause joint pains:
- Sarcoidosis, amyloidosis, and Whipple’s disease can also resemble RA.
- Hemochromatosis may cause hand joint arthritis.
- Acute rheumatic fever can be differentiated from RA by a migratory pattern of joint involvement and evidence of antecedent streptococcal infection. Bacterial arthritis (such as streptococcus) is usually asymmetric, while RA usually involves both sides of the body symmetrically.
- Gonococcal arthritis (another bacterial arthritis) is also initially migratory and can involve tendons around the wrists and ankles.
Prevention from Rheumatoid Arthritis
There is no known prevention for the contraction. Reduction of risk factors and aggressive treatment after diagnosis are recommended actions.
Treatment of Rheumatoid Arthritis
There is no cure for RA, but treatments can improve symptoms and slow the progress of the disease. Disease-modifying treatment has the best results when it is started early and aggressively.
The goals of treatment are to minimize symptoms such as pain and swelling, to prevent bone deformity (for example, bone erosions visible in X-rays), and to maintain day-to-day functioning. This can often be achieved using two main classes of medications: analgesics such as NSAIDs, and disease-modifying antirheumatic drugs (DMARDs). RA should generally be treated with at least one specific anti-rheumatic medication.
The use of benzodiazepines (such as diazepam) to treat the pain is not recommended as it does not appear to help and is associated with risks. Analgesics, other than NSAIDs, offer lesser, but some benefit with respect to pain. whilst not causing the same level of gastrointestinal irritation.
Lifestyle
Regular exercise is recommended as both safe and useful to maintain muscles strength and overall physical function. It is uncertain if specific dietary measures have an effect.
Disease modifying agents
Disease-modifying antirheumatic drugs (DMARD) are the primary treatment for RA. They are a diverse collection of drugs, grouped by use and convention. They have been found to improve symptoms, decrease joint damage, and improve overall functional abilities. They should be started very early in the disease as when they result in disease remission in approximately half of people and improved outcomes overall.
The most commonly used agent is methotrexate with other frequently used agents including sulfasalazine and leflunomide. Sodium aurothiomalate (Gold) and cyclosporin are less commonly used due to more common adverse effects. Agents may be used in combinations.
Methotrexate is the most important and useful DMARD and is usually the first treatment. Adverse effects should be monitored regularly with toxicity including gastrointestinal, hematologic, pulmonary, and hepatic. Side effects such as nausea, vomiting or abdominal pain can be reduced by taking folic acid. The most common undesirable affect is that it increases liver enzymes in almost 15% of people. It is thus recommended that those who consistently demonstrate abnormal levels of liver enzymes or have a history of liver disease or alcohol use undergo liver biopsies. Methotrexate is also considered a teratogenic and as such, it is recommended women of childbearing age should use contraceptives to avoid pregnancy and to discontinue its use if pregnancy is planned.
Biological agents should generally only be used if methotrexate and other conventional agents are not effective after a trial of three months. These agents include: tumor necrosis factor alpha (TNFα) blockers such as infliximab; interleukin 1 blockers such as anakinra, monoclonal antibodies against B cells such as rituximab, T cell costimulation blocker such as abatacept among others. They are often used in combination with either methotrexate or leflunomide.
TNF blockers and methotrexate appear to have similar effectiveness when used alone and better results are obtained when used together. TNF blockers appear to have equivalent effectiveness with etanercept appearing to be the safest. Abatacept appears effective for RA with 20% more people improving with treatment than without. There however is a lack of evidence to distinguish between the biologics available for RA. Issues with the biologics include their high cost and association with infections including tuberculosis.
Anti-inflammatory agents
NSAIDs reduce both pain and stiffness in those with RA. Generally they appear to have no effect on people’s long term disease course and thus are no longer first line agents. NSAIDs should be used with caution in those with gastrointestinal, cardiovascular, or kidney problems.
COX-2 inhibitors, such as celecoxib, and NSAIDs are equally effective. They have a similar gastrointestinal risk as an NSAIDs plus a proton pump inhibitor. In the elderly there is less gastrointestinal intolerance to celecoxib than to NSAIDs alone. There however is an increased risk of myocardial infarction with COX-2 inhibitors. Anti-ulcer medications are not recommended routinely but only in those high risk of gastrointestinal problems.
Glucocorticoids can be used in the short term for flare-ups, while waiting for slow-onset drugs to take effect. Injection of glucocorticoids into individual joints is also effective. While long-term use reduces joint damage it also results in osteoporosis and susceptibility to infections, and thus is not recommended.
Surgery
In early phases of the disease, an arthroscopic or open synovectomy may be performed. It consists of the removal of the inflamed synovia and prevents a quick destruction of the affected joints. Severely affected joints may require joint replacement surgery, such as knee replacement. Postoperatively, physiotherapy is always necessary.
Alternative medicine
There has been an increasing interest in the use of complementary and alternative medicine interventions for the treatment of pain in rheumatoid arthritis. While there have been multiple studies showing beneficial effects in RA on a wide variety of CAM modalities, these studies are often affected by publication bias and are generally not high quality evidence such as randomized controlled trials (RCTs), making definitive conclusions difficult to reach.
